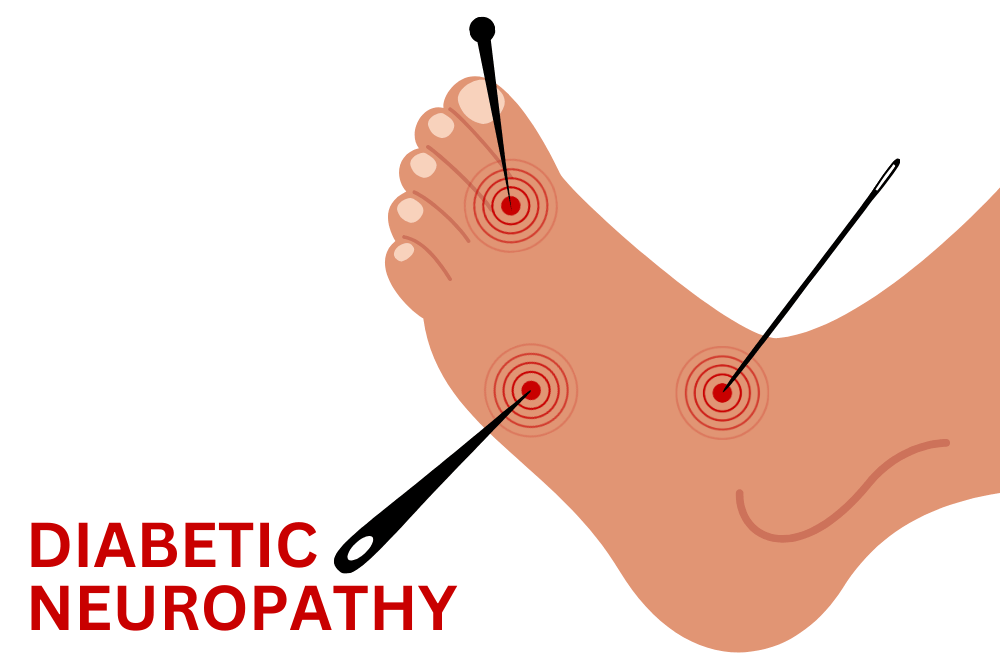
Diabetic neuropathy is a prevalent nerve impairment that can arise as a result of diabetes. Elevated blood sugar levels can inflict harm on nerves throughout the body. The nerve damage most frequently occurs in the legs and feet.
Diabetic neuropathy symptoms vary based on the affected nerves and may encompass sensations of pain and numbness in the legs, feet, and hands. This condition can also lead to complications in the digestive system, urinary tract, blood vessels, and heart. While some individuals experience mild symptoms, others grapple with intense pain and incapacitation.
A significant diabetes complication, diabetic neuropathy, affects potentially half of all diabetes patients. Nevertheless, consistent blood sugar management and a wholesome lifestyle can often forestall or decelerate the progression of this condition.
Symptoms and Variants
Diabetic neuropathy manifests in four primary types. It’s possible to encounter one or multiple variants of neuropathy.
The symptoms experienced hinge on the type of neuropathy and which nerves are compromised. Symptoms typically manifest progressively, and considerable nerve damage might occur before they become noticeable.
Peripheral Neuropathy
Commonly known as distal symmetric peripheral neuropathy, this type affects the extremities first—starting with the feet and legs, followed by the hands and arms. Symptoms, which can intensify during nighttime, encompass:
- Numbness or diminished sensitivity to pain or temperature changes
- Tingling or burning sensations
- Acute pains or cramps
- Muscle weakness
- Heightened sensitivity to touch, wherein even the weight of a bedsheet could be agonizing
- Severe foot issues, including ulcers, infections, and damage to bones and joints
Autonomic Neuropathy
The autonomic nervous system governs functions like blood pressure, heart rate, perspiration, eye function, bladder activity, digestion, and reproductive organs. Diabetes can impinge on nerves in these domains, resulting in signs such as:
- Reduced awareness of low blood sugar levels (hypoglycemia unawareness)
- Blood pressure drops upon transitioning from sitting or lying down, potentially causing dizziness or fainting (orthostatic hypotension)
- Impairment in bladder or bowel function
- Delayed stomach emptying (gastroparesis), leading to nausea, vomiting, a sense of fullness, and loss of appetite
- Difficulty in swallowing
- Altered adjustment of eyes to light-dark transitions and near-far focus
- Fluctuations in sweating patterns
- Disruptions in sexual response, such as vaginal dryness in females and erectile dysfunction in males
Proximal Neuropathy (Diabetic Polyradiculopathy)
This variant often affects nerves in the thighs, hips, buttocks, and legs, with potential influence on the abdominal and chest regions. Symptoms are usually unilateral but might extend to the opposite side and may include:
- Intense pain in the buttocks, hip, or thigh
- Weakening and atrophy of thigh muscles
- Difficulty in rising from a seated position
- Chest or abdominal wall pain
Mononeuropathy (Focal Neuropathy)
Mononeuropathy pertains to the impairment of a specific nerve. This nerve could be located in the face, torso, arm, or leg. Mononeuropathy can result in:
- Focus difficulties or double vision
- Facial paralysis on one side
- Tingling or numbness in the hand or fingers
- Hand weakness leading to dropped objects
- Shin or foot pain
- Weakness causing challenges in lifting the front of the foot (foot drop)
- Pain in the anterior thigh
When to Seek Medical Attention
Consult a healthcare professional if you experience:
- An infected or non-healing foot wound
- Discomfort, tingling, weakness, or pain in the feet or hands impeding daily life or sleep
- Alterations in digestive, urinary, or sexual function
- Episodes of dizziness and fainting
The American Diabetes Association recommends initiating diabetic neuropathy screening promptly after a type 2 diabetes diagnosis or five years following a type 1 diabetes diagnosis. Subsequent screenings should be conducted annually.
Causes and Risk Factors
The precise origins of each neuropathy type remain elusive. Experts speculate that prolonged unregulated high blood sugar inflicts damage on nerves, impairing their signal transmission abilities, thereby causing diabetic neuropathy. Moreover, heightened blood sugar weakens the walls of small blood vessels (capillaries) that provide oxygen and nutrients to nerves.
Certain factors increase the likelihood of nerve damage, including:
- Poor blood sugar management: Inadequate blood sugar control heightens the risk of all diabetes-related complications, including nerve damage.
- Diabetes duration: The risk of diabetic neuropathy escalates over time, particularly if blood sugar levels remain uncontrolled.
- Kidney dysfunction: Diabetes-induced kidney damage introduces toxins into the bloodstream, potentially causing nerve damage.
- Excess weight: A body mass index (BMI) of 25 or above raises the risk of diabetic neuropathy.
- Smoking: Smoking constricts and hardens arteries, diminishing blood flow to lower extremities. This impedes wound healing and damages peripheral nerves.
Complications and Consequences
Diabetic neuropathy can yield severe consequences:
- Impaired awareness of hypoglycemia: Individuals with autonomic neuropathy may not experience typical hypoglycemia symptoms when blood sugar drops below 70 mg/dL (3.9 mmol/L).
- Amputation risk: Nerve damage can dull sensation in the feet, rendering minor injuries potentially dangerous. Infections might escalate to bone involvement or tissue death, necessitating toe, foot, or leg amputation.
- Urinary tract issues and incontinence: Damaged bladder nerves can cause incomplete bladder emptying, fostering bacterial growth and urinary infections. Nerve damage might also hinder the sensation of needing to urinate or control over urine release, causing leakage.
- Sudden blood pressure drops: Nerve damage affecting blood flow regulation may lead to abrupt blood pressure declines upon standing, leading to lightheadedness and fainting.
- Gastrointestinal troubles: Digestive tract nerve damage may cause constipation, diarrhea, or gastroparesis, a condition where the stomach empties sluggishly or not at all, provoking bloating and indigestion.
- Sexual dysfunction: Autonomic neuropathy may compromise sexual organ nerves, causing erectile dysfunction in men and arousal/lubrication difficulties in women.
- Altered sweating patterns: Nerve damage can disrupt sweat gland function, jeopardizing body temperature regulation.
Prevention and Management of Diabetic Neuropathy
Diligent blood sugar control and foot care can mitigate diabetic neuropathy and its complications.
Blood Sugar Management
The American Diabetes Association advocates biannual glycated hemoglobin (A1C) tests for diabetes patients. This test measures average blood sugar levels over the past 2 to 3 months. While A1C goals may differ, maintaining an A1C level below 7.0% is often recommended. Modifications in medication, diet, or exercise may be needed if blood sugar levels deviate from the target.
Foot Care for Diabetic neuropathy
Foot problems associated with diabetic neuropathy can be averted through comprehensive foot exams at least annually. Regular foot checks during medical appointments and proper at-home care are crucial.
To ensure foot health:
- Keep your feet clean and dry by washing them daily with mild soap and lukewarm water. Thoroughly dry between toes to prevent moisture buildup.
- Moisturize your feet to prevent cracking, but avoid applying lotion between your toes to prevent fungal growth.
- Trim your toenails carefully, cutting them straight across and filing the edges to avoid sharp corners. Seek a podiatrist’s help if needed.
- Opt for clean, moisture-wicking socks made of cotton or suitable fibers that don’t constrict.
- Wear well-fitting, cushioned shoes that allow toe movement, helping to protect your feet. Consult a foot specialist to find appropriately fitted shoes and avoid problems like corns and calluses. Medicare plans might cover the cost of one pair of shoes per year if eligible.
By diligently managing blood sugar levels and practicing proper foot care, individuals can significantly reduce the risk of diabetic neuropathy and its associated complications. Regular medical check-ups, maintaining a healthy lifestyle, and adhering to medical advice also contribute to preventing the advancement of this condition.