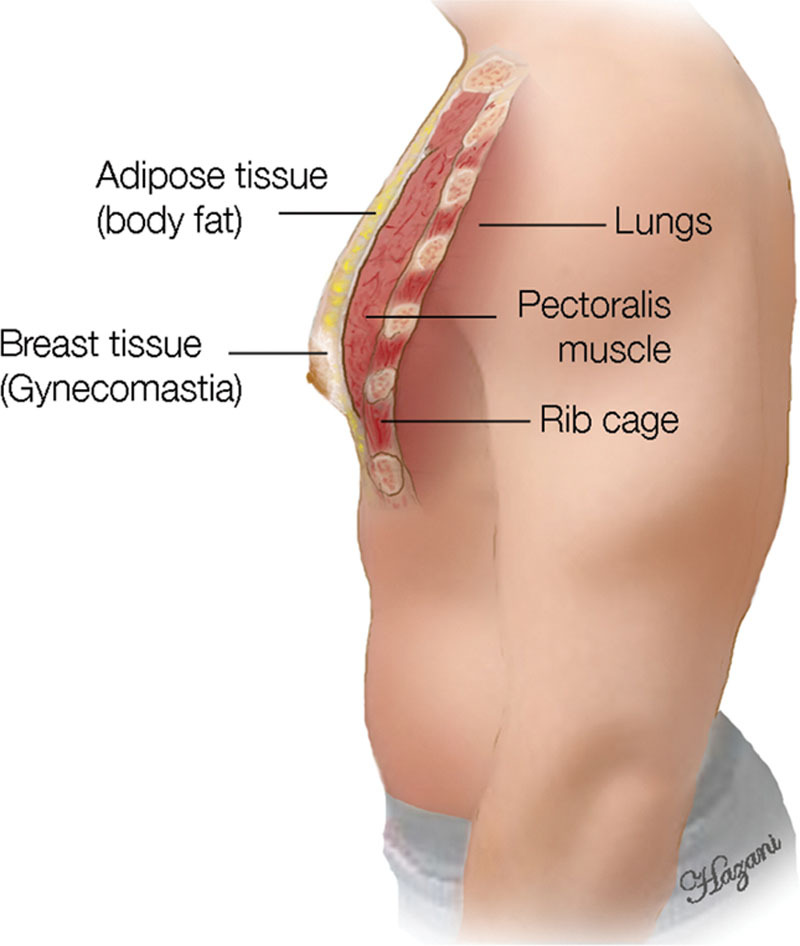
Gynecomastia, derived from Greek roots ‘gyne’ meaning women and ‘mastia’ referring to breast, manifests as an abnormal enlargement of breast tissue in males. This condition arises from an imbalance in testosterone and estrogen hormones, affecting males of any age, albeit more prevalent in children, adolescents, and the elderly.
Types of Gynecomastia:
Pseudo-gynecomastia: Primarily caused by excess fat accumulation in childhood, often manageable through lifestyle modifications without surgery.
Juvenile gynecomastia: Emerges during puberty, typically necessitating surgical intervention for resolution.
Drug-induced gynecomastia: Triggered by various medications or hormonal imbalances induced by dietary factors, typically requiring surgical correction.
Systemic disease gynecomastia: Arises from underlying complex medical conditions such as Klinefelter syndrome or liver cirrhosis.Grading and Risk Factors:
Gynecomastia severity is categorized into four grades based on breast tissue enlargement, with risk factors including aging, anabolic steroid use, liver or kidney disease, hormonal disorders, and substance abuse.
Symptoms and Diagnosis:
While many individuals with gynecomastia remain asymptomatic, common indications include breast pain, swelling, tenderness, and nipple discharge. Diagnosis involves thorough physical examination, medical history assessment, hormone level analysis, imaging tests such as ultrasound and mammography, and occasionally biopsy for cancer screening.
Treatment of Gynecomastia
Except for pseudo-gynecomastia, which may respond to lifestyle changes, surgical intervention is typically the primary treatment modality. Surgical procedures aim to remove excess breast tissue and reshape the chest contour, often yielding satisfactory aesthetic outcomes with minimal scarring.
In conclusion, understanding the multifaceted aspects of gynecomastia, from its etiology and classification to diagnosis and treatment options, is crucial for effective management and patient care.